Musculoskeletal disorders in patient handling
For the PDF version click here.
Prepared by: Carlo Caponecchia1 Robyn L. Coman2 Vinod Gopaldasani2 Elizabeth C. Mayland2 Luka Campbell3 1School of Aviation, The University of New South Wales, Sydney, Australia 2Occupational Health & Safety, School of Health & Society, University of Wollongong, NSW, 2522, Australia 3Centre for Work Health and Safety, NSW Department of Customer Service This is a preprint – the final accepted article is available from https://www.sciencedirect.com/science/article/pii/S0020748920302017
The article should be cited as: Caponecchia C., Coman, R.C., Gopaldasani, V., Mayland E. C., & Campbell, L. (2020). Musculoskeletal disorders in aged care workers: a systematic review of contributing factors and interventions. International Journal of Nursing Studies, 110, 103715https://doi.org/10.1016/j.ijnurstu.2020.103715 |
Executive summary
Background
There is limited evidence on contributing factors and effective interventions for musculoskeletal injuries in aged care workers.
Purpose
To systematically review the factors that contribute to musculoskeletal disorder risk amongst workers in the aged care industry, and to undertake a qualitative comparison of the interventions designed and implemented to prevent injury within this workforce.
Methods
A systematic review of the literature was conducted in Web of Science, Scopus, ProQuest, Medline, and PubMed. Relevant grey literature was also examined. Articles that reported factors that contribute to musculoskeletal injuries, or interventions to prevent and manage musculoskeletal injuries in residential aged care workers were included.
Findings
Of the 864 articles and 35 grey literature publications found, 63 and 29 were included in the review respectively. Results indicate that physical factors such as manual handling of people, use of assistive devices, and physical work environment are most commonly associated with musculoskeletal disorders in this population. Limited evidence of organisational and psychosocial factors considered staffing issues, work schedules, and violence. The heavy emphasis on physical factors is echoed in the grey literature in relevant guidance material and codes of practice focused on assessment and control of risks. There was limited evidence for interventions specific to aged care; existing evidence focused on equipment, training and education, policy and procedure. Interventions incorporating a combination of approaches, such as equipment and training, showed promise while preliminary evidence of the effectiveness of participatory approaches are positive.
Discussion
Interventions which address multiple types of contributing factors are needed to adequately prevent musculoskeletal injuries in aged care workers.
Key words: Aged care, musculoskeletal injuries, interventions, contributing factors
Introduction
Musculoskeletal disorders present a persistent and costly problem for society and contribute substantially to the global disease burden. The World Health Organisation (WHO) reports that musculoskeletal disorders are the leading contributor to disablement globally in all sectors (WHO, 2019) at an estimated cost in 2019 of $13.11 billion USD (Liberty Mutual, 2019). The incidence of musculoskeletal disorders is particularly high amongst healthcare workers, who may be exposed to a range of ergonomic hazards that interact in the causal pathway. In Australia, workers in the health and social assistance sector submit serious workers compensation claims more frequently than workers in any other sector. Within the sector, workers in the residential aged care industry experience the highest incidence of workers compensation claims (19.6 per million hours worked), and muscular stress is considered one of the main factors attributable to injury (Safe Work Australia, 2018). The term ‘residential aged care facilities’ typically excludes home-based care, community care, or supported living arrangements. In the United States (US), musculoskeletal disorder cases accounted for 31% of all lost-time worker injuries and illnesses in 2015, with healthcare designated as a high-risk sector for musculoskeletal disorders (US Bureau of Labour Statistics, 2015). Despite these alarming statistics, workers compensation datasets may represent only a fraction of the total disease burden of musculoskeletal disorders amongst healthcare workers. For example, Qin et al. (2014) found that less than 10% of nursing home workers with prevalent lower back pain actually submitted a claim.
Many authors have reported high prevalence of musculoskeletal disorders amongst nurses, nursing aides, and licenced practical nurses (Cohen-Mansfield, 1996; Davis & Kotowski, 2015; Hignett, 1996; Trinkoff, 2006). For instance, nursing is identified as one of the occupations at highest risk for back pain (Guo, 1995; Hignett, 1996), a form of musculoskeletal disorder, with up to 80% of nurses reporting back pain at some point in their lifetime (Hignett, 1996). In a more recent review, 55% of healthcare workers reported back pain in the past year (Davis & Kotowski, 2015). Unfortunately, the vast majority of this research has focused on nursing staff (including nursing aides) working in hospital settings, with very limited investigation of musculoskeletal disorders amongst workers in residential aged care facilities or home health settings (Davis & Kotowski, 2015; Sherehiy, Karwowski, & Marek, 2004; Simon, Tackenberg, Nienhaus, Estryn-Béhar, et al., 2008). The presentation of, and factors that contribute to musculoskeletal disorders in these settings are likely reflective of some of the unique characteristics and challenges of health care work.
Residential aged care facilities differ from hospital settings in some important ways. While hospitals focus on health needs of patients, residential aged care facilities provide care and accommodation for older adults who can no longer live independently in their own homes. People living in residential aged care facilities require assistance for most of their needs including activities of daily living, cognitive tasks, and administration of complex healthcare (Australian Institute of Health & Welfare, 2019). In contrast to hospitals, care at residential aged care facilities may be permanent or short-term respite, and may range from low care level (e.g. hostel) services to high care level nursing home services (Australian Institute of Health & Welfare, 2019). Direct care for residents is provided by aged care workers whose duties predominantly involve manual handling of people tasks. Care workers are therefore exposed to high frequency of manual handling of people tasks and associated ergonomic hazards (e.g. awkward posture, force, repetition), in meeting the care needs of older adults who may have varying, and fluctuating, levels of dependency. Compared to nurses working in hospitals, nurses working in residential care settings reported higher physical loads (32.2% vs 22.3%) and higher levels of disability (48.1% vs 44%) (Van der Heijden, Estryn-Béhar, & Heerkens, 2019). In addition, hazardous manual handling tasks are often performed in confined and/or cluttered spaces in resident’s bedroom and bathroom environments (Collins, Wolf, Bell, & Evanoff, 2004; Coman, Caponecchia, & McIntosh, 2018), and under time constraints arising from inadequate or insufficient staffing (e.g. during periods of peak load) (Trinkoff, 2006). Further compounding musculoskeletal disorder risk for aged care workers is resident related factors such as behaviours associated with cognitive impairment (e.g. combativeness), patient obesity (Gallagher, 2005) and the risk of a resident falling (Collins et al., 2004; Zhang, Punnett, & Gore, 2014).
Theoretical frameworks can be useful for describing the phenomena that contribute to musculoskeletal disorder aetiology, so that theoretically grounded interventions can be developed. Typically, such frameworks have distinguished between physical, organisation and psychosocial risk factors, while postulating that these risk factors often interact in the causal pathway thereby giving effect to multifactorial aetiology (Carayon, Haims, Hoonakker, & Swanson, 2006; Oakman, Macdonald, Bartram, Keegel, & Kinsman, 2018). Physical factors refer to the nature of tasks (pulling, pushing, lifting, moving), the nature and quantity of loads manipulated in those tasks, and the features of the physical environment and equipment available. Organisational factors are those variables that management of the organisation control through regular business management systems and processes (Macdonald & Oakman, 2013). These include the structure of the organisation (e.g. hierarchies, governance, responsibilities and accountabilities), the human resources and employment practices used (e.g. contractual arrangements, shift rosters and length), the resourcing of the facility and procurement issues, the leadership styles, commitment to safety, and culture and values of the workplace. Psychosocial factors are aspects of the physical and social environment that can have an effect on mental processes such as thoughts, attitudes, expectations, perceptions, motivations, emotions, as well as on behaviours (Caponecchia, 2018; Martikainen, Bartley, & Lahelma, 2002). Physical, organisational and psychosocial factors clearly overlap and interact with one another in any work environment. For this reason, it can sometimes be difficult to isolate the factors from one another, or to make clear distinctions on which made a more significant contribution to a particular outcome.
Within the aged care context, physical factors have long been identified as the principal contributing risk factor for musculoskeletal disorders amongst nursing and care staff (Engkvist, Hagberg, Hjelm, Menckel, & Ekenvall, 1998; Hignett, 1996; Stubbs, Buckle, Hudson, Rivers, & Worringham, 1983). These factors are exemplified by manual handling of people tasks such as assisting patients/residents with transferring to or from furniture, repositioning in bed and performing daily hygiene tasks (e.g. bathing, toileting), the lifting equipment and assistive devices used to assist with these tasks, the environments in which these tasks occur (e.g. bedrooms, bathrooms) and the type, design and/or adjustment of available equipment and furniture (e.g. adjustable or non-adjustable beds and chairs) (Coman et al., 2018). Other factors associated with musculoskeletal disorder aetiology amongst nurses include long working hours (Trinkoff, 2006), stressful working conditions and poor workplace culture (Bernal, 2015; Daraiseh, 2003), poor communication between colleagues (Andersen, Vinstrup, Villadsen, Jay, & Jakobsen, 2019) and organisational changes such as an increase to patient loads (Lipscomb, 2004). In aged care, additional factors such as the (low) social value associated with aged care work may play into the psychosocial factors on the job (Isherwood, Mavromaras, Moskos, & Wei, 2018; Siewert, 2017). For example, the way in which a job is viewed can influence who takes such roles, why they take such roles, and how they view the importance, responsibility or contribution of what they do. This may be able to be countered or influenced by organisational actions but may not be directly related to organisational factors in the way that other psychosocial factors are.
Although a number of contributing factors have been identified, there is limited information about the effectiveness of interventions designed to prevent musculoskeletal disorders or address the pain and disability experienced by healthcare workers. The paucity of information available has either been of poor quality or tended to focus on single interventions such as training in the manual handling of people (Richardson, McNoe, Derrett, & Harcombe, 2018). However, the failure of traditional manual
handling of people interventions to decrease the incidence of musculoskeletal disorders among healthcare workers support that the factors that contribute to the development of musculoskeletal disorders in these workers are multifactorial. This review aims to systematically review the factors that contribute to musculoskeletal disorder risk amongst workers in the aged care industry, to highlight the application of this evidence related to these factors in relevant grey literature, and to undertake a qualitative comparison of the interventions designed and implemented to prevent injury within this population.
Methodology
The search strategy for this systematic review was developed by the research team in consultation with staff from the Centre for Workplace Health and Safety (New South Wales Department of Customer Service). The databases searched comprised Web of Science, Scopus, ProQuest, Medline and PubMed. Search inclusion criteria comprised that the record be peer-reviewed and in English, and that it not be an editorial, letter or commentary, a magazine article, or case law. Grey literature was considered in additional searches (described below). The scope of the review was limited to aged care homes (residential aged care facilities or RACFs), excluding home-based care, community care, or supported living arrangements. The focus was on outcomes for workers rather than on outcomes for residents/patients.
Searches for factors contributing to musculoskeletal disorders in aged care combined ‘outcome terms’ with ‘target terms’ and ‘modifiers’ of each target term. Outcome terms comprised: musculoskeletal disorder OR low back disorders OR low back pain OR nurse injur* OR care worker injur* OR back injur* OR shoulder injur* OR upper limb injur* OR repetit* strain injur* OR strain injur*. These were combined with ‘target terms’: “aged care OR elder care OR nursing home OR residential care OR residential aged care OR aged care institution OR aged care facility OR home for the aged” and ‘modifiers of target terms’: “staff OR aide* OR worker* OR assistant OR carer*†”.1,2
Searches for musculoskeletal disorder interventions combined all the search terms above with ‘intervention terms’: “intervention* OR prevention OR training OR risk control OR risk prevention OR injury prevention OR reducing injur* OR improving health OR safe* OR risk management OR manual handling” and ‘modifiers of ‘intervention terms’: “strateg* OR program* OR plan* OR system* OR protocol*”. Each of the intervention terms were joined with each of the modifiers.
The search and screening process was conducted in the stages outlined in the PRISMA model, from identification, screening, eligibility and inclusion (Liberati et al., 2009). A rubric for exclusion of records
1 The symbol ‘*’ indicates wildcard or truncations, so that, for example, injur* captures injury, injuries, injured.
2 The symbol ‘†’ indicates modifying terms that were only used with the following target terms: nursing home, aged care institution, aged care facility and home for the aged. was used by members of the research team to screen out records before reading the full text. All proposed inclusions and exclusions of records were checked by at least two team members. Records found in the search process may have focused on topics that were outside the scope of this review. In addition to the general inclusion/exclusion criteria outlined above, records which focused on the following topics were excluded: oral health; patient care outcomes/satisfaction; dementia care; palliative care decisions; decisions for transfer to hospital; resident pressure injury management; family member perspectives; childhood; medicines; patient mental health; incontinence; viral transmission, vaccination; elder abuse; patient pain assessment; community nursing/outreach; and natural disasters.
The final set of records was divided between the research team to read in full and assess in relation to the factors contributing to musculoskeletal disorders in aged care, and interventions that could be employed. The PRISMA diagram in Figure 1 indicates the number of records excluded at each stage of the process, and the resulting number of articles included in the review.
Grey literature, such as government and industry publications and guidance, position papers, as well as contract research reports can form an important part of the evidence base in applied fields. The grey literature relevant to musculoskeletal disorder causation (generally and for aged care specifically), and interventions to prevent musculoskeletal disorders was sourced from government and industry publications and guidance material, position papers, contract research reports, and literature identified in reference lists of articles that were selected for inclusion. Of the 35 publications identified, six were excluded as they were not directly relevant to musculoskeletal disorders.
In addition, a qualitative framework for classifying levels of evidence as outlined by Reay, Berta and Kohn (2009) was employed in relation to intervention studies. The levels of evidence from Reay et al can be summarised as follows:
Level 1. Large Randomised Control Trials (RCT) and meta-analyses
Level 2. High quality literature reviews and smaller RCTs
Level 3. Comparative, multisite case studies or large sample quantitative studies (e.g. with samples from several organisations); prospective cohort studies
Level 4. Smaller sample, single-site qualitative or quantitative studies
Level 5. Descriptive or self-report studies, including observations
Level 6. Studies based on subject matter expert views; anecdotal evidence
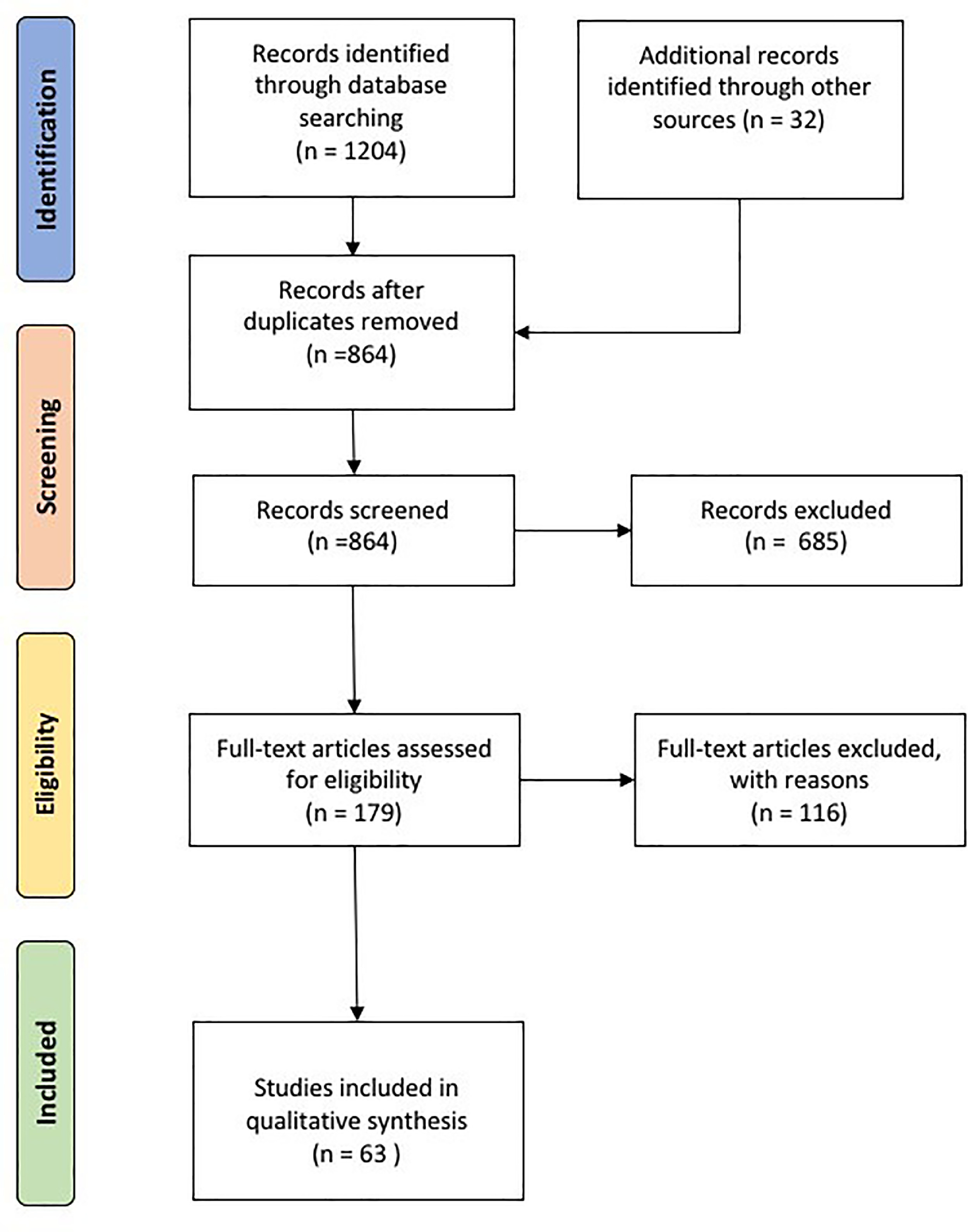
Figure 1 – PRISMA diagram outlining the search results regarding factors contributing to musculoskeletal disorders in the aged care industry and associated interventions.
Results
Factors contributing to musculoskeletal disorders in aged care
Physical factors
The earliest factors associated with musculoskeletal disorders in aged care workers were physical factors. Personick (1990) reported that 15 workplace injuries were recorded per 100 full-time equivalent (FTE) staff in nursing home aides. The majority of these injuries were musculoskeletal disorder related, and physical factors were primarily identified as the main contributing factor to the occurrence of musculoskeletal disorders. These included tasks associated with assisting the resident resulting in trunk and back injuries that constituted 61% of all injuries. Myers et al. (1994) confirmed these findings among nursing home aides and attributed the injuries to a lack of lifting equipment and often working alone when conducting such tasks. Physical ergonomic interventions were thus suggested as an effective intervention strategy to assist with pushing, pulling and lifting activities (A. Myers, Jensen, Nestor, & Rattiner, 1994). The National Institute for Occupational Safety and Health (NIOSH) further evaluated nursing assistants in aged care homes and identified eight stressful tasks that contributed to musculoskeletal disorders. These included (1) lifting up in bed, (2) transferring from bed to wheel chair, (3) transferring from wheelchair to bed, (4) transferring from wheelchair to toilet, (5) transferring toilet to wheelchair, (6) transferring from bathtub/shower to wheelchair, (7) transferring from chair lift to wheelchair, and (8) weighing residents. Interestingly, nursing assistants performed an average of 24 of these tasks per eight-hour shift without assistive devices (Collins & Owen, 1996). The focus was on the lack of assistive devices that contributed to musculoskeletal disorders mainly as a result of overexertion and falls by care workers (Meyer & Muntaner, 1999). A study of palliative care workers showed that almost 50% of the staff had suffered a musculoskeletal disorder, mainly lower back injury, in the previous one year of working (Smith, Guo, Lee, & Chang, 2002). Tasks linked to these injuries included changing residents’ clothes (OR = 2.9, 95% CI [1.4, 6.3]), changing bed linens with residents still on the bed (OR = 2.8, 95% CI [1.4, 6.1]), and moving residents in and out of the bed (OR = 2.5, 95% CI [1.2, 5.4]) all without any assistive devices. For facilities that did have assistive devices, lack of maintenance of these devices has also been associated with improper use or failed use and thus associated with musculoskeletal disorders (Ching et al., 2018; Robertson, 1999; Scott, Pokorny, Rose, & Watkins, 2010). Other devices apart from assistive devices include appropriate seating to aid sit-to-stand transfers that require minimal lifting effort on the part of the carers (Coman et al., 2018). Features of the physical work environment have also been associated with musculoskeletal disorders especially slips, trips and falls which can subsequently result in other musculoskeletal disorders (Bell et al., 2013). These features include wet floors, loose wires, objects on the floor, surface irregularities and inadequate lighting (Mughal, 2005). Task frequency is another physical factor that was positively correlated with musculoskeletal disorders in aged care, as increased frequency of tasks during a shift is a major factor for multiple recurrent injuries including musculoskeletal disorders (Oranye, 2018).
The ubiquitous presence and emphasis on physical factors in research studies was also reflected in the grey literature analysis. For instance, the NSW Code of Practice for Hazardous Manual Tasks (SafeWork NSW, 2016), based on the Model Code of Practice for Hazardous Manual Tasks developed by SafeWork Australia (2011), provides guidance on the identification, assessment and control of risks associated with hazardous manual tasks. The majority of this guidance is focused on the risk assessment of physical factors within the domains of postures and movements which includes pushing, pulling and lifting activities, forces exerted which includes exertional, rotational and torsional forces and environmental which includes aspects of the physical environment which are unrelated to aged care settings. Similarly, Workplace Health & Safety Queensland (2001) produced a Code of Practice specifically related to manual handling of people, entitled Manual tasks involving the handling of people Code of Practice 2001 (Workplace Health and Safety Queensland, 2001). The Code considers physical factors as in the NSW Code of Practice, organisational factors, and to a lesser extent psychosocial musculoskeletal disorder risk factors and includes extensive information and practical tools for managing manual handling of people risks.
In addition to the codes of practices, a range of grey literature included manual handling of people guides which focuses on patient/resident risk assessments and transfer guides. These guides clearly focus on the physical factors discussed. Examples of such guides include the WorkSafe Victoria ‘Transferring People Safely’ Guide 3rd Edition (WorkSafe Victoria, 2009) and the Queensland Health (2012) Patient Handling Facility Unit Risk Assessment Tool (FURAT). Safe systems for manual handling of people task performance have been developed for application in other countries, including New Zealand (Accident and Compensation Commission New Zealand, 2012; Thomas & Thomas, 2012; Work Safe New Zealand, 2018), the USA (Department of Veteran Affairs, 2005; National Institute for Occupational Safety and Health [NIOSH], 2019; A. L. Nelson, 2005; Occupational Safety and Health Administration [OSHA], 2009), Canada (Interior Health, 2019) and the United Kingdom (Wilford, 2012). The ISO Technical Report ISO/TR 12296:2012 Ergonomics. Manual handling of people in the healthcare sector, provides comprehensive guidance on manual handling of people assessment and risk control, including reference to a range of patient handling assessment tools that can be applied for quantification of injury risk exposure (International Organisation for Standardisation [ISO], 2012). These tools predominantly focus on physical factors and include the web-based Care Thermometer tool (Huntleigh, 2019) for evaluation of overall risk levels within a work unit through assessment of patient dependency levels, tasks, equipment and some environmental factors.
Organisational factors
The most prevalent organisational factor that has been associated with musculoskeletal disorders in care workers is inadequate staffing levels (Castle, Engberg, Mendeloff, & Burns, 2009; Ching et al., 2018; Park, Bushnell, Bailer, Collins, & Stayner, 2009; Scott et al., 2010; Trinkoff, Johantgen, Muntaner, & Le, 2005). Low staff to resident ratios has consistently been associated with an increased risk of musculoskeletal disorders as this results in increased task frequency, longer shift hours, longer working week and fatigue all of which add to the increasing risk of musculoskeletal disorders. The second most prevalent organisational factor identified was leadership behaviours, styles and attitude to the workplace and the care workers (Backman, Sjögren, Lindkvist, Lövheim, & Edvardsson, 2016; Backman, Sjögren, Lövheim, & Edvardsson, 2018; Ching et al., 2018; Haas, Hunter, & Howard, 2018). Organisational management demonstrated through leadership styles and attitudes were most often in direct contradiction to the health and safety of the carers (Haas et al., 2018). This in turn manifested in a lack of or poor induction to the workplace, education and training, communication, culture and policy (Banaszak-Holl et al., 2017; Ching et al., 2018; Haas et al., 2018; Myers, Silverstein, & Nelson, 2002; Nelson et al., 2006; Patterson, 1993; Robertson, 1999; Stanev et al., 2012). These organisational factors are all crucial to ensure a duty of care to the aged care workers by management.
Analysis of the grey literature showed minimal incorporation of organisational factors into Codes of Practice and guidance documents. The Workplace Health & Safety Queensland Code of Practice was the only Code that addressed organisational factors extensively. This included workloads, shift duration and frequency of shifts, staffing levels, training programs and policies and procedures. Of relevance to this review, the ISO/TR 12296:2012 extends the focus on physical risk factors evident in the vast majority of guidance publications, through specific consideration of the importance of organisational aspects of manual handling of people interventions, such as management commitment to resources.
Psychosocial factors
Psychosocial factors associated with musculoskeletal disorders are more difficult to identify as they tend to overlap with physical and organisational factors. Fatigue, shift work and poor posture have been associated with the occurrence of low back pain (Kai, 2001). These factors are clear examples of overlap between the physical, organisational and psychosocial factors associated with musculoskeletal disorders. Violence from residents suffering dementia as well as from family members has also been identified as a psychosocial factor contributing to musculoskeletal disorders in aged care (Åkerström, 2002; Brodaty, Draper, & Low, 2003). However, there is disagreement on the use of the term “violence” as opposed to “aggression” whereby carers may rationalise otherwise violent behaviours and outbursts as acts of unintended aggression, thus falling outside the boundary of “violence” per se in this particular work context (Åkerström, 2002). High or increasing job demands is another psychosocial factor associated with musculoskeletal disorders (Backman et al., 2018; Chang et al., 2013; Gold, Kurowski, Gore, Punnett, & ProCare Research Team, 2018; Gold, Punnett, Gore, & ProCare Research Team, 2017), particularly in relation to back and shoulder injuries (Myers et al., 2002). In the study by Myers et al. (2002), carers who cared for a greater number of residents, which meant that they performed more strenuous tasks per shift, were associated with a modest increase in risk of injuries. Furthermore, new employees due to rapid staff turnover were also significantly at risk of injuries (OR = 2.55, 95% CI [1.04, 6.26]). High job demands and job strains are also psychosocial factors associated with musculoskeletal disorders (Backman et al., 2018; Chang et al., 2013; Gold et al., 2018; Gold et al., 2017). Again, it is important to note that job demands and job strains also overlap with organisational factors, as organisational leadership, culture and support closely influence job demands and strain (Backman et al., 2018; Banaszak-Holl et al., 2017; Haas et al., 2018). The lack of social support and poor social integration from colleagues and the organisation at large have also been associated with musculoskeletal disorders in aged care staff and some research indicates that these psychosocial factors are critical predictors of musculoskeletal disorders (Backman et al., 2018; Gold et al., 2018; Myers et al., 2002). Interpersonal conflicts and poor working relationships between care workers and between care workers and residents are also psychosocial factors associated with musculoskeletal disorders. These are sometimes identified as “indirect” contributors to injury, through lack of cooperation, assistance or neglect when performing high risk tasks (Graham & Dougherty, 2012; Payne & Appel, 2007). Lastly, effort-reward imbalance, work-life imbalance and work-family conflicts are now recognised psychosocial contributors to musculoskeletal disorders in aged care workers (Pelissier et al., 2014; Simon, Tackenberg, Nienhaus, Estryn-Behar, et al., 2008; Weale, Wells, & Oakman, 2018). Pelissier et al. (2014) identified a work imbalance of long shifts per day as being more associated with musculoskeletal disorders than a long working week. Trinkoff et al (2005) also reported this and in addition reported that weekend work, off-shift work, and overtime were associated risk factors for musculoskeletal disorders but also highlighted that these perceived psychosocial factors were significantly overlapping with physical factors and demands associated with such work schedules.
A review of the grey literature highlighted the complex interplay of physical and psychosocial musculoskeletal disorder risk factors, that is of relevance to manual handling of people related injuries within the health, community and aged care sectors (Belardi, 2014; McMillan, Moo, Newman, & Da Silva, 2018; Oakman & Kinsman, 2016; Shea et al., 2016). Belardi (2014) reviews several investigations of aged care staff injuries, highlighting the need to consider worker ‘wellbeing’ with a focus on the individual. An audit of manual handling of people systems identified evidence of multi-factor interventions (McMillan et al. 2018) within health care and ambulance services. Barriers to effective manual handling of people practice included organisational and psychosocial factors (e.g. management commitment; resources for equipment, training and staff; training effectiveness; staff turnover). Findings of Oakman et al’s (2016) investigation of musculoskeletal disorder risk management in 19 organisations (10 logistics/transport and 9 aged care) was consistent with the aforementioned review of guidance on the manual handling of people. They reported that the key barriers to musculoskeletal disorder prevention included: beliefs that musculoskeletal disorder risks are principally physical; musculoskeletal disorder policies, procedures and guidance that focus on physical risk factors; and strategies to manage psychosocial risks mainly target individual behaviours with limited consideration of organisational and psychosocial hazards.
Interventions for musculoskeletal disorders in the aged care industry
There is limited research specific to the residential aged care sector exploring the effectiveness of interventions designed to reduce musculoskeletal disorders. Most (14) of the articles in the review that considered interventions were categorised as Level 4 (small sample, single-site qualitative or quantitative studies) according to the Reay, Berta and Kohn (2009) levels of evidence classifications. Six articles were at Level 3 (comparative, multisite case studies or large sample quantitative studies), two articles were at Level 5 (anecdotal evidence and subject matter expert views), and only one record was at Level 2 (high quality literature reviews and small randomised control trials).
The literature that does focus on aged care describes interventions that generally fall into the following categories: equipment-based interventions, training/education, procedural or policy changes, and multi-dimensional intervention approaches. The vast majority of studies included a combination of approaches. This makes it difficult to determine the relative effectiveness of any one component of the intervention or to make generalisations about any one approach.
The use of lifting equipment showed generally positive effects on the rate of injury among aged care workers. Regardless of type of equipment used, Anderson (2014) found that the use of an assistive device during transfers provided a protective effect from injury for those who performed transfers on a daily basis (Andersen et al., 2014). The benefits of one particular type of lift over another is unclear. Miller et al. (2006) found that overhead lifts incorporated into the design of a new facility resulted in a significant reduction in injuries and improved perceptions of safety when compared both to levels of injury prior to moving into a new facility and to a control facility using mechanical lifts only (Miller, 2006). However, the purchase of smaller scale ergonomic lifting equipment (such as lifts or electric beds) that can be incorporated in existing facilities also has a beneficial effect (Park et al., 2009). Mechanical lifts have been found to be effective at significantly reducing injuries, most often in conjunction with employee training on use of lifts (Collins & Owen, 1996; Collins et al., 2004) and a zero-lift policy (Collins & Owen, 1996; Collins et al., 2004; Stanev et al., 2012). Some systems (such as the Columbus McKinnon Assist Personal Transfer System) resulted in less strain on users than others (such as the Hoyer lift), potentially contributing to lower injury rates (Gingher, 1996). However, other studies have shown no improvement in injury rates with any particular piece of equipment (Stanev et al., 2012). The majority of these studies incorporated training in the use of equipment with the introduction of these equipment, suggesting that training may be a mediator of the effectiveness of equipment in reducing injury rates.
Lifting equipment used in conjunction with other interventions shows promise. The implementation of a “no lift” policy in combination with provision of appropriate equipment and staff training on use of the equipment shows consistently positive results on injury rates (Pocock, 2004; Rockefeller, Silverstein, & Howard, 2000; Stanev et al., 2012). Black et al (2011) found that a combination of staff education, equipment, and procedures to identify individual patient needs related to transfers decreased staff injury (Black et al., 2011). Adding some modification of the environment (e.g. to toilets or showers to improve access) to this combination also reduced injury rates (Garg, 1992). As described in a narrative review by Coman et al. (2018) environmental modifications which improve a patient’s independence with mobility may also be effective in reducing injury rates as they decrease the manual handling load on care workers.
Training alone has mixed effectiveness within the aged care sector. No improvement in low back pain (Jensen et al., 2006) was found following training in patient handling techniques alone. Education in patient handling combined with stress management techniques (Peterson, McGlothlin, & Blue, 2004) or effective communication techniques (Mughal, 2005) also provided no improvement in injury, although the focus on communication did appear to improve the safety climate of the organisation overall (Mughal, 2005). Physical training, on the other hand, might provide some protective effect. In a laboratory study, Pederson et al. (2007) demonstrated that employees of a geriatric ward retained learning from training designed to elicit more protective physical responses to unexpected trunk perturbations for up to 1 year following training (Pedersen et al., 2007). This skill may be beneficial to care workers who perform transfers with patients, where unexpected movements from the individual being transferred are common.
Interventions designed to address organisational factors have also been beneficial. Selecting appropriate staff members following physical evaluation and creating a specially trained “lift team,” who received training in biomechanics, proper use of equipment, assessment of patient for transfers, warm-up and stretching exercises, completing daily lift logs, and ongoing support by the trainer resulted in high satisfaction by other team members and minimal injuries reported during the study (Caska, Patnode, & Clickner, 1998). Staffing levels are significantly correlated with injury rates, with a decrease in worker injury rates of 2 per 100 FTEs shown for every unit increase in staffing (Trinkoff et al., 2005). As noted above, a focus on administrative changes such as the implementation of a “no lift” policy or managerial support of specific policies around manual handling are also effective when used in combination with additional factors such as equipment and staff training.
There is limited but promising evidence on the use of participatory ergonomics in the aged care sector. Preliminary evidence indicates that this may be an effective intervention for injury reduction in this environment. Udo, Kobayashi, Udo, and Branlund (2006) demonstrated a reduction in general musculoskeletal disorders in care staff and cooks within the aged care sector following an intervention involving staff identification of problematic tasks resulting in identification and modification of tasks that placed the most stress on the lower back (Udo et al., 2006). However, due to the individual nature of this type of intervention, further research is required to determine effectiveness and generalisability.
Discussion
This review aimed to examine two main issues in relation to musculoskeletal disorders in the aged care industry: a) the factors that contribute to musculoskeletal disorders in aged care workers, and b) the interventions used to decrease the rate of musculoskeletal disorders in the aged care industry.
Overall, we found that while physical, organisational and psychosocial factors have been found to contribute to musculoskeletal disorders in aged care, the interventions used did not always address multiple types of contributing factors. Psychosocial contributors tended to be less well addressed in interventions, while physical contributors were more likely to be featured among interventions (e.g. through lifting equipment, training in relation to lifting equipment; training in musculoskeletal disorders and ergonomics generally). Contributing factors that are categorised as organisational affect physical and psychosocial factors and potential interventions, but interventions that function at an organisational level (such as through leadership development, resourcing, procurement and culture) were relatively scarce. The quality of evidence was not particularly high, with most articles on interventions being small sample and single site qualitative and quantitative work, as opposed to larger cohort studies or high-quality literature reviews.
These findings were reflected in the grey literature, where physical contributing factors were the main focus. Despite some consideration of organisational contributors to musculoskeletal disorders in the ISO technical report, ISO/TR 12296:2012, it is recognised that across various industries the understanding of the contribution of psychosocial and organisational factors to musculoskeletal disorders is limited (Oakman & Kinsman, 2016). In parallel, while there are a number of publications providing guidance to employers for interventions designed to manage these physical risks, there is limited guidance for managing the contribution of psychosocial and organisational factors.
That interventions tended to not be psychosocial in nature does not mean that they could not or did not have psychosocial implications or effects. All workplace safety interventions arguably have a (positive or negative) psychosocial effect. For example, lifting equipment provision can communicate commitment of the organisation to safety, as can the quality and nature of training programs or other interventions. Participative interventions may affect psychosocial aspects of work by their nature, for example, through encouraging collaboration and consultation they may enhance perceptions of control and decision latitude, perceived organisational support, and perceptions of leadership and safety culture/climate. Nonetheless, the interventions found in the review tended to not have a focus on changing psychosocial elements of the work organisation or tasks, nor a theory of change based on, or inclusive of, psychosocial attributes.
A range of issues appear to have made communication of the interplay of physical, organisational and psychosocial factors in musculoskeletal disorders challenging. These factors have not always been defined, or consistently defined. The lack of definition is exacerbated by the factors being interdependent. It can be difficult to distinguish factors of a particular type from one another when they may have multiple outcomes that appear associated with another factor (e.g. an organisational factor of resourcing producing a psychosocial outcome such as low perceived support). In addition, communication about the mechanisms by which psychosocial and organisational factors may affect musculoskeletal disorders have not always been clear or relatable for industry, nor indicative of the range of ways in which these factors can have an effect (e.g. by affecting tasks). Psychosocial factors, in particular, are known to be poorly understood and inconsistently communicated about, across a range of stakeholders (Johnstone, Quinlan, & McNamara, 2011; Leka, Van Wassenhove, & Jain, 2015; Lippel & Quinlan, 2011). They are sometimes viewed as being related only to mental health or psychological injury outcomes, rather than contributing to other injury outcomes, or affecting other hazards more generally. This problem reflects a wider knowledge gap in safety more generally, rather than being unique to musculoskeletal disorders.
Macro-focused interventions may be required to improve safety literacy for industry, regulators and safety professionals. This in turn may advance the consideration of the full range of contributing factors when designing and implementing interventions. While not a conventional musculoskeletal disorder intervention, this kind of strategy is needed to provide a foundation for any other intervention to be implemented successfully, with adequate resources and ongoing support.
None of the literature reviewed considered environmental interventions for musculoskeletal disorders in aged care, consistent with the findings of Coman et al. (2018). Risk assessment for environmental factors were mentioned in the grey literature. However, as outlined in the introduction, the aged care industry has unique features that distinguish it from healthcare operations and may therefore warrant interventions that are appropriately differentiated and environmentally specific. For example, features of the main hazardous manual tasks are different to manual tasks in many other industries (e.g. lifting and moving older people, who may have cognitive decline, and may exhibit violence). The manual handling of people raises important challenges in this workplace context, including the changing nature of care needs (from high to low care areas in a facility), the ability of the resident to assist with lifting/moving, and their level of mobility, both of which may change within a matter of hours. Accordingly, features of the aged care facility environment, can be very important for reducing the manual handling of people task load. This can manifest in a number of ways, including facilitating the use of lifting equipment by staff, facilitating the use of assistive equipment by residents, and facilitating the mobility of the residents themselves so they can assist in the transfer. Relevant environmental features, as identified by Coman et al (2018) include bed, chair and toilet height and adjustability; assistive technology to aid mobility; clear space for care staff, residents, and equipment, including space around the bed and fixed architectural features, and room dimensions and room access. Optimising environmental factors to improve mobility of older adults within manual handling of people risk management in aged care is a higher-level risk control strategy in terms of effectiveness and warrants further attention in research and practice.
While evidence for participative ergonomics interventions in preventing musculoskeletal disorders is mixed, they are commonly used in other settings and have a greater chance of addressing a wider range of contributing factors than other interventions (Burgess-Limerick, 2018). Consideration should be given to tailored participative ergonomics programs in the aged care sector. Importantly, this should include facilitation of involvement from a range of staff members (including senior management and board members) so that organisational factors might be discussed and addressed. Rather than using participation and consultation to improve known or existing interventions (such as manual handling training), a participative approach might be used to identify wider system factors that contribute to musculoskeletal disorders. In this way a more collaborative, system-based intervention which is tailored to a specific aged care residential facility could be developed, which responds to the full range of factors that contribute to musculoskeletal disorders.
As mentioned above, all interventions can have a psychosocial impact without necessarily being focused on psychosocial changes. For instance, staffing is a major issue that deserves further attention as it directly impacts on the efficacy of all musculoskeletal disorder interventions in aged care. Far from just being about requiring more staff, issues of valuing aged care work in the community, through remuneration, esteem, professional development and career opportunities also need to be considered. This could contribute to retaining staff, as well as fostering positive and supportive workplace environments, where job satisfaction, commitment and perception of contribution are high (Fedele, 2019).
Another high level and long-term intervention with psychosocial implications that may assist with a number of problems in the aged care industry is a program of career development and education. Such a program might include opportunities for education in occupational health and safety, management and clinical skills; mentoring, the identification of career progression pathways and increased renumeration with skill development. This kind of program may not specifically target musculoskeletal disorder prevention per se but would target issues including a lack of career development, the hierarchical nature of aged care work, and the perception of aged care work being under-valued, as well as developing team and industry leaders with safety knowledge and competencies (Dwyer, 2011; King, 2012). In this way, the workplaces taking up such a program would be transformed, leading to greater job retention, satisfaction and commitment; safety leadership and skills, and mentorship for new workers, who would also have opportunities for career progression. Other musculoskeletal disorder prevention strategies would therefore be implemented in facilitative environments, with leadership, relevant safety competencies and commitment.
This review was limited in scope to aged care facilities and did not consider home care or community-based care. It was not the intention of this review to function as a meta-analysis – indeed, it was not intended to focus on the efficacy of interventions. Nonetheless, some commentary on the efficacy of interventions has been presented, rather than a simple list of possible interventions.
Conclusion
Findings from this review of peer reviewed and grey literature extends existing knowledge, in clearly identifying the current status of musculoskeletal disorder evidence and published musculoskeletal disorder risk management guidance, relevant to musculoskeletal disorder prevention within residential aged care. Organisational and psychosocial musculoskeletal disorder causation does not appear to have been comprehensively considered within the sector. The complex interplay between physical, organisational and psychosocial musculoskeletal disorder risk factors in aged care warrants proactive, and long-term education and awareness interventions from collaborations between industry, researchers and regulators. Building on this critical base, there are opportunities to tailor existing multidimensional and participatory interventions to aged care, alongside new safety frameworks and tools, as well as to develop context specific environmental strategies that can improve safety for all stakeholders in aged care.
References
Accident and Compensation Commission New Zealand. (2012). Moving and handling people. The New Zealand Guidelines. Retrieved from https://www.acc.co.nz/assets/provider/1d98940288/acc6075-moving-and-handling-peopleguidelines.pdf
Åkerström, M. (2002). Slaps, punches, pinches-but not violence: Boundary-work in nursing homes for the elderly. Symbolic Interaction, 25(4), 515-536. doi:10.1525/si.2002.25.4.515
Andersen, L. L., Burdorf, A., Fallentin, N., Persson, R., Jakobsen, M. D., Mortensen, O. S., . . . Holtermann, A. (2014). Patient transfers and assistive devices: prospective cohort study on the risk for occupational back injury among healthcare workers. Scand J Work Environ Health, 40(1), 74-81. doi:10.5271/sjweh.3382
Andersen, L. L., Vinstrup, J., Villadsen, E., Jay, K., & Jakobsen, M. D. (2019). Physical and Psychosocial Work Environmental Risk Factors for Back Injury among Healthcare Workers: Prospective Cohort Study. Int J Environ Res Public Health, 16(22). doi:10.3390/ijerph16224528
Australian Institute of Health & Welfare. (2019). Aged care: Snapshot. Retrieved from https://www.aihw.gov.au/reports/australias-welfare/aged-care
Backman, A., Sjögren, K., Lindkvist, M., Lövheim, H., & Edvardsson, D. (2016). Towards personcentredness in aged care -exploring the impact of leadership. Journal Of Nursing Management, 24(6), 766-774. doi:10.1111/jonm.12380
Backman, A., Sjögren, K., Lövheim, H., & Edvardsson, D. (2018). Job strain in nursing homes-Exploring the impact of leadership. Journal Of Clinical Nursing, 27(7-8), 1552-1560. doi:10.1111/jocn.14180
Banaszak-Holl, J., Reichert, H., Todd Greene, M., Mody, L., Wald, H. L., Crnich, C., . . . Meddings, J. (2017). Do Safety Culture Scores in Nursing Homes Depend on Job Role and Ownership? Results from a National Survey. Journal Of The American Geriatrics Society, 65(10), 22442250. doi:10.1111/jgs.15030
Belardi, L. (2014). Special report: staff injuries in aged care. Australian Ageing Agenda. Retrieved from https://www.australianageingagenda.com.au/2014/11/26/special-report-staff-injuriesagedcare/
Bell, J. L., Collins, J. W., Tiesman, H. M., Ridenour, M., Konda, S., Wolf, L., & Evanoff, B. (2013). Slip, trip, and fall injuries among nursing care facility workers. Workplace Health & Safety, 61(4), 147-152. doi:10.3928/21650799-20130318-28
Bernal, D., Campos-Serna, J., Tobias, A., et al. (2015). Work-related psychosocial risk factors and musculoskeletal disorders in hospital nurses and nursing aides: a systematic review and meta-analysis. International Journal Of Nursing Studies, 52, 635-648. doi: http://dx.doi.org/10.1016/j.ijnurstu.2014.11.003
Black, T. R., Shah, S. M., Busch, A. J., Metcalfe, J., & Lim, H. J. (2011). Effect of Transfer, Lifting, and Repositioning (TLR) Injury Prevention Program on Musculoskeletal Injury Among Direct Care Workers. Journal of Occupational & Environmental Hygiene, 8(4), 226-235. doi:10.1080/15459624.2011.564110
Brodaty, H., Draper, B., & Low, L.-F. (2003). Nursing home staff attitudes towards residents with dementia: strain and satisfaction with work. Journal Of Advanced Nursing, 44(6), 583-590. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=mnh&AN=14651681&site=ehost-live
Burgess-Limerick, R. (2018). Participatory ergonomics: Evidence and implmentation lessons. Applied Ergonomics, 68, 289-293.
Caponecchia, C. (2018). Towards Integration: Psychosocial issues and MSDs. Paper presented at the Keynote address Safework NSW Musculoskeletal Disorders Symposium 8-9 November 2018 Sydney.
Carayon, P., Haims, M. C., Hoonakker, P. L. T., & Swanson, N. G. (2006). Teamwork and musculoskeletal health in the context of work organization interventions in office and computer work. Theoretical Issues in Ergonomics Science, 7(1), 39-69. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106441426&site=ehost-live
Caska, B. A., Patnode, R. E., & Clickner, D. (1998). Feasibility of a nurse staffed lift team. AAOHN Journal, 46(6), 283-288. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=107281169&site=ehost-live
Castle, N. G., Engberg, J., Mendeloff, J., & Burns, R. (2009). A national view of workplace injuries in nursing homes. Health Care Management Review, 34(1), 92-103. doi:10.1097/01.HMR.0000342981.37673.74
Chang, V., Hiller, C., Keast, E., Nicholas, P., Su, M., & Hale, L. (2013). Musculoskeletal disorders in support workers in the aged care sector. Physical Therapy Reviews, 18(3), 185-206. doi:10.1179/1743288X13Y.0000000083
Ching, S. S. Y., Szeto, G., Lai, G. K. B., Lai, X. B., Chan, Y. T., & Cheung, K. (2018). Exploring the Synergic Effects of Nursing Home Work on Work-Related Musculoskeletal Disorders Among Nursing Assistants. Workplace Health & Safety, 66(3), 129-135. doi:10.1177/2165079917717497
Cohen-Mansfield, J., Culpepper, W.J., Carter, P. (1996). Nursing staff back injuries: prevalence and cost in long term care facilities. AAOHN Journal, 44, 9-17.
Collins, J. W., & Owen, B. (1996). NIOSH research initiatives to prevent back injuries to nursing assistants, aides, and orderlies in nursing homes. American Journal Of Industrial Medicine, 29(4), 421-424. doi:10.1002/(sici)1097-0274(199604)29:4<421::Aid-ajim30>3.0.Co;2-1
Collins, J. W., Wolf, L., Bell, J., & Evanoff, B. (2004). An evaluation of a “best practices” musculoskeletal injury prevention program in nursing homes. Injury Prevention, 10(4), 206211.
Coman, R. L., Caponecchia, C., & McIntosh, A. S. (2018). Manual Handling in Aged Care: Impact of Environment-related Interventions on Mobility. Safety and Health at Work, 9(4), 372-380. doi:10.1016/j.shaw.2018.02.003
Daraiseh, N., Genaidy, A.M., Karwowski, W., et al. (2003). Musculoskeletal outcomes in multiple body regions and work effects among nurses: the effects of stressful and stimulating working conditions. Ergonomics, 46, 1178-1199. doi:http://dx.doi.org/10.1080/0014013031000139509
Davis, K. G., & Kotowski, S. E. (2015). Prevalence of Musculoskeletal Disorders for Nurses in Hospitals, Long-Term Care Facilities, and Home Health Care: A Comprehensive Review. Hum Factors, 57(5), 754-792. doi:10.1177/0018720815581933
Department of Veteran Affairs. (2005). Patient Care Ergonomics Resource Guide: Safe Patient Handling & Movement. Retrieved from https://osha.oregon.gov/edu/grants/train/Documents/va-patient-care-ergonomicsresourceguide-part-1-rev-8-2005.pdf
Dwyer, D. (2011). Experiences of registered nurses as managers and leaders in residential aged care facilities: a systematic review. International Journal of Evidence-Based Healthcare, 9(4), 388402.
Engkvist, I. L., Hagberg, M., Hjelm, E. W., Menckel, E., & Ekenvall, L. (1998). The accident process preceding overexertion back injuries in nursing personnel. PROSA study group. Scand J Work Environ Health, 24(5), 367-375.
Fedele, R. (2019). Aged care workers underpaid, undervalued and short-staffed, Royal Commission told. Australian Nursing and Midwifery Journal. Retrieved from https://anmj.org.au/agedcare-workers-underpaid-undervalued-and-short-staffed-royal-commission-told/
Gallagher, S. (2005). Obesity and the aging adult: ideas for promoting patient safety and preventing caregiver injury. Clinics In Geriatric Medicine, 21(4), 757. Retrieved from https://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=16182088&site=ehost-live
Garg, A., Owen, B. (1992). Reducing back stress in nursing personnel: an ergonomic intervention in a nursing home. Ergonomics, 35(11), 1353-1375.
Gingher, M., J. Karuza, et al. (1996). Effectiveness of lift systems for long term care residents. Physical & Occupational Therapy in Geriatrics, 13(2), 1-11.
Gold, J. E., Kurowski, A., Gore, R. J., Punnett, L., & ProCare Research Team (2018). Knee pain in nursing home workers after implementation of a safe resident handling program. American Journal Of Industrial Medicine, 61(10), 849-860. doi:10.1002/ajim.22902
Gold, J. E., Punnett, L., Gore, R. J., & ProCare Research Team (2017). Predictors of low back pain in nursing home workers after implementation of a safe resident handling programme. Occupational And Environmental Medicine, 74(6), 389-395. doi:10.1136/oemed-2016103930
Graham, P., & Dougherty, J. P. (2012). Oh, their aching backs!: occupational injuries in nursing assistants. Orthopaedic Nursing, 31(4), 218-223. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=108144419&site=ehost-live
Guo, H. R., Tanaka, S., Cameron, L.L., et al., . (1995). Back pain among workers in the United States: national estimates and workers at high risk. American Journal Of Industrial Medicine, 28, 591-602.
Haas, A. D., Hunter, D. A., & Howard, N. L. (2018). Bringing a structural perspective to work: Framing occupational safety and health disparities for nursing assistants with work-related musculoskeletal disorders. Work, 59(2), 211-229. doi:10.3233/WOR-172676
Hignett, S. (1996). Work-related back pain in nurses. Journal Of Advanced Nursing, 23(6), 1238-1246.
Huntleigh, A. (2019). The Care Thermometer. Retrieved from https://www.arjo.com/int/solutions/programmes/care-thermometer/
Interior Health. (2019). Safe Patient Handling. Retrieved from https://www.interiorhealth.ca/sites/Partners/WHSresources/Pages/SafePatientHandling.aspx
International Organisation for Standardisation [ISO]. (2012). ISO/TR 12296: Ergonomics. Manual handling of people in the healthcare sector. In (Vol. 12296). Geneva, Switzerland.
Isherwood, L., Mavromaras, K., Moskos, M., & Wei, Z. (2018). Attraction, Retention and Utilisation of the Aged Care Workforce. Canberra Retrieved from https://agedcare.health.gov.au/sites/default/files/documents/09_2018/retention_and_utilisation_of_the_aged_care_workforce_uni.of_adelaide_-_20.4.18.pdf
Jensen, L. D., Gonge, H., Jørs, E., Ryom, P., Foldspang, A., Christensen, M., . . . Bonde, J. P. (2006). Prevention of low back pain in female eldercare workers: randomized controlled work site trial. Spine (03622436), 31(16), 1761-1769. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106165326&site=ehost-live
Johnstone, R., Quinlan, M., & McNamara, M. (2011). OHS inspectors and psychosocial risk factors: Evidence from Australia. Safety Science, 49, 547-557.
Kai, S. (2001). Consideration of low back pain in health and welfare workers. Journal of Physical Therapy Science, 13(2), 149-152. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106816835&site=ehost-live
King, D. (2012). It's frustrating! Managing emotional dissonance in aged care work. Australian Journal of Social Issues, 47(1), 51-70.
Leka, S., Van Wassenhove, W., & Jain, A. (2015). Is psychosocial risk prevention possible? Deconstructing common presumptions. Safety Science, 71, 61-67.
Liberati, A., Altman, D., Tetzlaff, J., Mulrow, C., Gøtzsche, P., & al., e. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. British Medical Journal, 339(b2700). doi:10.1136/bmj.b2700
Liberty Mutual. (2019). 2019 Liberty Mutual Workplace Safety Index. Retrieved from https://business.libertymutualgroup.com/businessinsurance/Documents/Services/DS200.pdf
Lippel, K., & Quinlan, M. (2011). Regulation of psychosocial risk factors at work: An international overview. Safety Science, 49, 543-546.
Lipscomb, J., Trinkoff, A., Brady, B., et al. . (2004). Health care system changes and reported musculoskeletal disorders among registered nurses. American Journal of Public Health, 94, 1431-1435.
Macdonald, W., & Oakman, J. (2013). Musculoskeletal Disorders at work: Using evidence to guide practice. J Health & Safety Research & Practice, 5(2), 7-12.
Martikainen, P., Bartley, M., & Lahelma, E. (2002). Psychosocial determinants of health in social epidemiology. In: Oxford University Press.
McMillan, J., Moo, A., Newman, S., & Da Silva, A. (2018). Improvements in patient handling for worker and patient safety. Current and emerging approaches for worker and patient safety interventions. Retrieved from WorkSafe Victoria: https://research.iscrr.com.au/__data/assets/pdf_file/0004/1321771/EnvironmentalScan_Improvements-in-patient-handling-for-worker-and-patient-safety.pdf
Meyer, J. D., & Muntaner, C. (1999). Injuries in home health care workers: An analysis of occupational morbidity from a state compensation database. American Journal Of Industrial Medicine, 35(3), 295-301. doi:10.1002/(sici)1097-0274(199903)35:3<295::Aid-ajim10>3.3.Co;2-r
Miller, A., Engst, C., Tate, R.B., & Yassi, A. (2006). Evaluation of the effectiveness of portable ceiling lifts in a new long-term care facility. Applied Ergonomics, 37(3), 377-385.
Mughal, W. A. (2005). Assessment of low back injury risk in residential care workers. (M.Sc.). Simon Fraser University (Canada), Ann Arbor. ProQuest Dissertations & Theses Global database. (MR03543)
Myers, A., Jensen, R. C., Nestor, D., & Rattiner, J. (1994). Low Back Injuries Among Home Health Aides Compared With Hospital Nursing Aides. Home Health Care Services Quarterly, 14(2-3), 149-155. doi:10.1300/J027v14n02_11
Myers, D., Silverstein, B., & Nelson, N. A. (2002). Predictors of shoulder and back injuries in nursing home workers: A prospective study. American Journal Of Industrial Medicine, 41(6), 466476. doi:10.1002/ajim.10076
National Institute for Occupational Safety and Health [NIOSH]. (2019). Safe Patient Handling Resources. Retrieved from https://www.cdc.gov/niosh/topics/safepatient/
Nelson, A., Matz, M., Chen, F., Siddharthan, K., Lloyd, J., & Fragala, G. (2006). Development and evaluation of a multifaceted ergonomics program to prevent injuries associated with patient handling tasks. International Journal Of Nursing Studies, 43(6), 717-733. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true &db=rzh&AN=106332767&site=ehost-live
Nelson, A. L. (2005). Safe patient handling and movement: A practical guide for health care professionals: Springer Publishing Company.
Oakman, J., & Kinsman, N. (2016). Workplace barriers to reducing the incidence of musculoskeletal and mental health disorders. Retrieved from ISCRR: https://research.iscrr.com.au/__data/assets/pdf_file/0015/751002/Workplace-barriers-toreducing-the-incidence-of-musculo.skeletal-and-mental-health-disorders.pdf
Oakman, J., Macdonald, W., Bartram, T., Keegel, T., & Kinsman, N. (2018). Workplace risk management practices to prevent musculoskeletal and mental health disorders: What are the gaps? Safety Science, 101, 220-230. doi:https://doi.org/10.1016/j.ssci.2017.09.004
Occupational Safety and Health Administration [OSHA]. (2009). Guidelines for nursing homes: Ergonomics for the prevention of musculoskeletal disorders. Retrieved from https://www.osha.gov/ergonomics/guidelines/nursinghome/final_nh_guidelines.pdf
Oranye, N. O. (2018). Nature of Injury and Risk of Multiple Claims Among Workers in Manitoba Health Care. Workplace Health & Safety, 66(2), 70-83. doi:10.1177/2165079917728942
Park, R. M., Bushnell, P. T., Bailer, A. J., Collins, J. W., & Stayner, L. T. (2009). Impact of Publicly Sponsored Interventions on Musculoskeletal Injury Claims in Nursing Homes. American Journal Of Industrial Medicine, 52(9), 683-697. doi:10.1002/ajim.20731
Patterson, D. C. (1993). Minimizing back injuries in nursing home staff. Nursing Homes, 42(5), 20.
Payne, B. K., & Appel, J. K. (2007). Workplace violence and worker injury in elderly care settings: reflective of a setting vulnerable to elder abuse? Journal of Aggression, Maltreatment & Trauma, 14(4), 43-56. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=105915477&site=ehost-live
Pedersen, M. T., Essendrop, M., Skotte, J. H., Jorgensen, K., Schibye, B., & Fallentin, N. (2007). Back muscle response to sudden trunk loading can be modified by training among healthcare workers. Spine (Phila Pa 1976), 32(13), 1454-1460. doi:10.1097/BRS.0b013e318060a5a7
Pelissier, C., Fontana, L., Fort, E., Agard, J. P., Couprie, F., Delaygue, B., . . . Charbotel, B. (2014). Occupational Risk Factors for Upper-limb and Neck Musculoskeletal Disorder among Healthcare Staff in Nursing Homes for the Elderly in France. Industrial Health, 52(4), 334-346. doi:10.2486/indhealth.2013-0223
Personick, M. E. (1990). Nursing home aides experience increase in serious injuries. Monthly Labor Review, 113(2), 30-37. Retrieved from https://search.proquest.com/docview/79681046?accountid=12763
http://primoa.library.unsw.edu.au/openurl/61UNSW_INST/UNSW_SERVICES_PAGE?url_ver=Z39.882004&rft_val_fmt=info:ofi/fmt:kev:mtx:journal&genre=article&sid=ProQ:ProQ%3Atoxline&atitle=Nursing+home+aides+experience+increase+in+serious+injuries.&title=Monthly+labor+review&issn=00981818&date=1990-0201&volume=113&issue=2&spage=30&au=Personick%2C+M+E&isbn=&jtitle=Monthly+labor+review&btitle=&rft_id=info:eric/10170521&rft_id=info:doi/
Peterson, E. L., McGlothlin, J. D., & Blue, C. L. (2004). Ergonomics. The development of an ergonomics training program to identify, evaluate, and control musculoskeletal disorders among nursing assistants at a state-run veterans' home. Journal of Occupational & Environmental Hygiene, 1(1), D10-16. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106684196&site=ehost-live
Pocock, M., Bonner, R. (2004). Implementing no lift no injury in the aged care sector. Retrieved from Qin, J., Kurowski, A., Gore, R., & Punnett, L. (2014). The impact of workplace factors on filing of workers' compensation claims among nursing home workers. BMC Musculoskeletal Disorders, 15(1), 29-29. doi:10.1186/1471-2474-15-29
Reay, T., Berta, W., & Kohn, M. K. (2009). What's the Evidence on Evidence-Based Management? Academy of Management Perspectives, 23(4), 5-18. doi:10.5465/amp.23.4.5
Richardson, A., McNoe, B., Derrett, S., & Harcombe, H. (2018). Interventions to prevent and reduce the impact of musculoskeletal injuries among nurses: A systematic review. International Journal Of Nursing Studies, 82, 58-67.
Robertson, H. (1999). Pre-employment screening for aged care workers: a post injury follow-up. Geriaction, 17(4), 5-10. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true &db=rzh&AN=107079924&site=ehost-live
Rockefeller, K., Silverstein, B., & Howard, N. (2000). Getting to zero-lift in Washington State nursing homes. Paper presented at the Proceedings of the Human Factors and Ergonomics Society Annual Meeting.
Safe Work Australia. (2018). Priority Industry Snapshot: Healthcare and Social Assistance. Retrieved from https://www.safeworkaustralia.gov.au/doc/health-care-and-social-assistance-priorityindustry-snapshots-2018
SafeWork NSW. (2016). Code of Practice for Hazardous Manual Tasks. NSW Government Retrieved from https://www.safework.nsw.gov.au/__data/assets/pdf_file/0020/50078/hazardousmanual-tasks-code-of-practice-0916.pdf
Scott, E. S., Pokorny, M. E., Rose, M. A., & Watkins, F. (2010). Safe 'handoffs' for the morbidly obese. Bariatric Nursing & Surgical Patient Care, 5(1), 71-74. doi:10.1089/bar.2009.9935
Shea, T., De Cieri, H., Sheehan, C., Donohue, R., Cooper, B. J. V. I. f. s., compensation, & research, r. (2016). Occupational health and safety issues for aged care workers: A comparison with public hospital workers.
Sherehiy, B., Karwowski, W., & Marek, T. (2004). Relationship between risk factors and musculoskeletal disorders in the nursing profession: A systematic review. Occupational Ergonomics, 4, 241-279.
Siewert, R. (2017). Future of Australia's Aged Care Sector Workforce: Community Affairs References Committee.
Simon, M., Tackenberg, P., Nienhaus, A., Estryn-Behar, M., Conway, P. M., & Hasselhorn, H. (2008). Back or neck-pain-related disability of nursing staff in hospitals, nursing homes and home care in seven countries--results from the European NEXT-Study. International Journal Of Nursing Studies, 45(1), 24-34. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=105839725&site=ehost-live
Simon, M., Tackenberg, P., Nienhaus, A., Estryn-Béhar, M., Conway, P. M., & Hasselhorn, H. M. (2008). Back or neck-pain-related disability of nursing staff in hospitals, nursing homes and home care in seven countries—Results from the European Next-Study. International Journal Of Nursing Studies, 45, 24-34. doi:https://doi.org/10.1016/j.ijnurstu.2006.11.003
Smith, D. R., Guo, Y. L., Lee, Y., & Chang, S. (2002). Ergonomic and demographic issues reported by palliative care workers in southern Taiwan. American Journal of Hospice & Palliative Care, 19(2), 96-91p. Retrieved from http://ezproxy.uow.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=106836858&site=ehost-live
Stanev, S., Bailer, A. J., Straker, J. K., Mehdizadeh, S., Park, R. M., & Li, H. J. (2012). Worker Injuries and Safety Equipment in Ohio Nursing Homes. Journal Of Gerontological Nursing, 38(6), 4756. doi:10.3928/00989134-20120508-01
Stubbs, D. A., Buckle, P. W., Hudson, M. P., Rivers, P. M., & Worringham, C. J. (1983). Back pain in the nursing profession. I. Epidemiology and pilot methodology. Ergonomics, 26(8), 755-765. doi:10.1080/00140138308963397
Thomas, D., & Thomas, Y. (2012). Guidelines for moving and handling people in home care: New Zealand. Retrieved from https://www.mhanz.org.nz/wpcontent/uploads/2018/01/Microsoft-Word-Moving-Handling-People-Home-care-2012.pdf
Trinkoff, A. M. (2006). Musculoskeletal problems of the neck, shoulder, and back and functional consequences in nurses. American Journal Of Industrial Medicine, 41(3), 170-178. doi:10.1002/ajim.10048
Trinkoff, A. M., Johantgen, M., Muntaner, C., & Le, R. (2005). Staffing and worker injury in nursing homes. American Journal of Public Health, 95(7), 1220-1225. doi:10.2105/AJPH.2004.045070
Udo, H., Kobayashi, M., Udo, A., & Branlund, B. (2006). Participatory ergonomic improvement in nursing home. Ind Health, 44(1), 128-134.
US Bureau of Labour Statistics. (2015). Nonfatal Occupational Injuries and Illnesses Requiring Days Away From Work, 2015 [Press release]. Retrieved from https://www.bls.gov/news.release/osh2.nr0.htm
Van der Heijden, B., Estryn-Béhar, M., & Heerkens, H. (2019). Prevalence of, and risk factors for, physical disability among nurses in Europe. Open Journal of Social Sciences, 7, 147-173. doi:https://doi.org/10.4236/jss.2019.711012
Weale, V. P., Wells, Y., & Oakman, J. (2018). Self-reported musculoskeletal disorder pain: The role of job hazards and work-life interaction. American Journal Of Industrial Medicine, 61(2), 130139. doi:10.1002/ajim.22793
WHO. (2019). Musculoskeletal Conditions. Retrieved from https://www.who.int/news-room/factsheets/detail/musculoskeletal-conditions
Wilford, J. (2012). The Guide to the Handling of People: A Systems Approach. Occupational Medicine, 62(4), 310-310. doi:10.1093/occmed/kqs012 %J Occupational Medicine
Work Safe New Zealand. (2018). Moving and handling people in the healthcare industry. Retrieved from https://worksafe.govt.nz/topic-and-industry/health-and-safety-in-healthcare/movingandhandling-people-in-the-healthcare-industry/
Workplace Health and Safety Queensland. (2001). Manual tasks involving the handling of people Code of Practice. Retrieved from https://www.worksafe.qld.gov.au/__data/assets/pdf_file/0007/58174/manual-taskspeoplehandling-cop-2001.pdf
WorkSafe Victoria. (2009). Transferring people safely. Retrieved from https://www.worksafe.vic.gov.au/resources/transferring-people-safely-handbookworkplaces
Zhang, Y., Punnett, L., & Gore, R. (2014). Relationships among employees' working conditions, mental health, and intention to leave in nursing homes. Journal Of Applied Gerontology: The Official Journal Of The Southern Gerontological Society, 33(1), 6-23. doi:10.1177/0733464812443085
